Tuberculosis
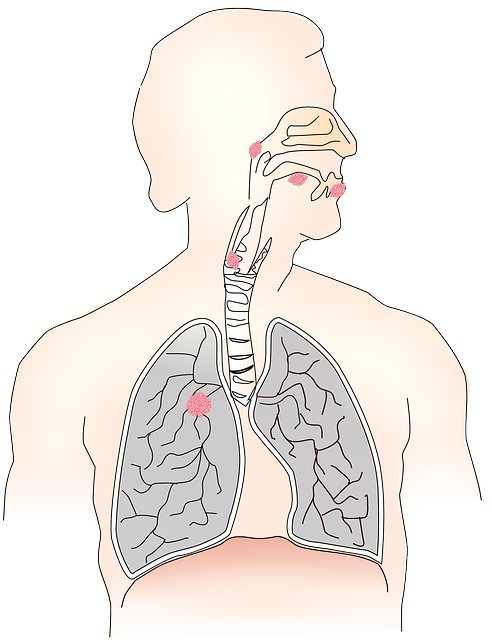
Tuberculosis (TB) remains one of the world’s most pressing health issues, despite significant advances in medical science. This infectious disease, caused by the bacterium Mycobacterium tuberculosis, primarily affects the lungs but can also impact other parts of the body. Understanding the nature of TB, its transmission, symptoms, diagnosis, and treatment options is crucial in the global fight against this formidable disease.
Understanding Tuberculosis
What is Tuberculosis?
Tuberculosis is a contagious bacterial infection that can spread through the air when a person with active TB of the lungs or throat coughs, sneezes, or talks. Unlike many bacterial infections, TB can lie dormant in the body for years. There are two forms of TB: latent TB infection and active TB disease.
- Latent TB Infection: Individuals with latent TB carry the bacteria but do not exhibit symptoms and cannot transmit the disease. However, the bacteria can become active, making it crucial to monitor and manage latent TB to prevent future outbreaks.
- Active TB Disease: This form occurs when the immune system cannot contain the bacteria, leading to symptoms and the potential to spread the infection to others.
How is TB Transmitted?
TB is primarily transmitted through airborne particles. When someone with active pulmonary TB coughs or sneezes, tiny droplets containing the bacteria are released into the air. If another person inhales these droplets, they can become infected. Factors influencing TB transmission include:
- Proximity to an Infected Person: Close and prolonged contact increases the risk.
- Ventilation: Enclosed spaces with poor ventilation facilitate the spread.
- Immune System Health: Individuals with weakened immune systems, such as those with HIV/AIDS, diabetes, or malnutrition, are more susceptible to TB infection.
Symptoms of Tuberculosis
The symptoms of TB can vary depending on whether it is latent or active and the part of the body affected. However, pulmonary TB, which affects the lungs, is the most common form. Key symptoms include:
- Persistent Cough: Lasting more than three weeks, often producing phlegm and sometimes blood.
- Chest Pain: Especially when breathing or coughing.
- Fatigue: Persistent tiredness and weakness.
- Fever: Low-grade fevers are common.
- Night Sweats: Profuse sweating during sleep.
- Weight Loss: Unintended and significant loss of weight.
- Loss of Appetite: Reduced desire to eat.
Extrapulmonary TB, which affects other organs, may present with symptoms related to the infected area, such as back pain (spinal TB) or swelling of lymph nodes (lymphatic TB).
Diagnosing Tuberculosis
Early diagnosis of TB is essential for effective treatment and prevention of transmission. Several diagnostic methods are available:
Tuberculin Skin Test (TST)
The Mantoux tuberculin skin test involves injecting a small amount of tuberculin into the skin of the forearm. After 48-72 hours, the injection site is examined for a reaction. A raised, hard area may indicate TB infection, but false positives can occur in people who have received the BCG vaccine or have been exposed to non-TB mycobacteria.
Interferon-Gamma Release Assays (IGRAs)
Blood tests such as the QuantiFERON-TB Gold and T-SPOT.TB measure the immune system’s response to TB bacteria. These tests are more specific than the TST and are less likely to give false-positive results in individuals vaccinated with BCG.
Chest X-rays and CT Scans
Imaging techniques help detect lung abnormalities indicative of TB. While these methods do not confirm TB, they are useful in identifying signs that warrant further testing.
Sputum Tests
Microscopic examination and culture of sputum samples are critical for confirming pulmonary TB. These tests can detect TB bacteria and determine if they are resistant to specific drugs.
Molecular Tests
Nucleic acid amplification tests (NAATs) such as the Xpert MTB/RIF assay can detect TB bacteria and resistance to rifampicin, a key TB drug, within a few hours. These tests are highly sensitive and specific.
Treatment of Tuberculosis
Treating TB involves a combination of antibiotics taken over an extended period. The treatment regimen depends on whether the TB is drug-sensitive or drug-resistant.
Drug-Sensitive TB
The standard treatment for drug-sensitive TB is a 6-month course of antibiotics, typically including:
- Isoniazid
- Rifampicin
- Ethambutol
- Pyrazinamide
The initial phase lasts two months and includes all four drugs. The continuation phase lasts four months, with isoniazid and rifampicin.
Drug-Resistant TB
Multidrug-resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB) are more challenging to treat due to resistance to first-line drugs. Treatment often involves second-line drugs, which may be less effective, more toxic, and require longer treatment durations, typically 18-24 months.
Newer drugs such as bedaquiline and delamanid have shown promise in treating MDR-TB, offering hope for better outcomes.
Treatment Adherence
Adherence to the full course of treatment is crucial to cure TB and prevent the development of drug-resistant strains. Directly observed therapy (DOT) is a strategy where healthcare providers supervise patients taking their medications, ensuring adherence and monitoring side effects.
Prevention of Tuberculosis
Preventing TB involves multiple strategies, including vaccination, screening, and public health measures.
BCG Vaccine
The Bacillus Calmette-Guérin (BCG) vaccine provides some protection against severe forms of TB in children. However, its effectiveness in preventing pulmonary TB in adults is limited, and it is not widely used in countries with a low prevalence of TB.
Screening and Prophylaxis
Screening high-risk populations, such as people with HIV, healthcare workers, and close contacts of TB patients, helps identify and treat latent TB infection, preventing progression to active disease.
Infection Control
In healthcare settings, implementing airborne precautions, such as the use of N95 respirators and proper ventilation, helps reduce the risk of TB transmission. Public health initiatives aimed at improving living conditions, nutrition, and access to healthcare are vital in reducing TB incidence.
Public Awareness and Education
Raising awareness about TB symptoms, transmission, and the importance of completing treatment is essential in controlling the spread of TB. Public education campaigns can reduce stigma and encourage individuals to seek medical help early.
Challenges in TB Control
Despite advances in TB diagnosis and treatment, several challenges remain:
- Drug Resistance: The emergence of MDR-TB and XDR-TB complicates treatment and requires significant resources.
- HIV Co-infection: People with HIV are at higher risk of developing TB, and TB is a leading cause of death among those with HIV/AIDS.
- Funding and Resources: TB control programs require sustained funding and resources to be effective, particularly in low- and middle-income countries.
- Stigma: Stigma associated with TB can deter individuals from seeking diagnosis and treatment.
Conclusion
Tuberculosis continues to pose a significant global health challenge, requiring a multifaceted approach for effective control. Early diagnosis, appropriate treatment, prevention strategies, and public awareness are critical components in the fight against TB. With concerted efforts from governments, healthcare providers, and communities, it is possible to reduce the burden of TB and move closer to a world free of this ancient disease.